Taking Care of Healthcare Workers
How on-the-job respite improves clinician wellbeing and ROI.
It’s a troubling paradox: The wellbeing of healthcare workers — whose jobs are centered on taking good care of others — is all too often overlooked in their own work environments.
Compared to people in other professions, those who work in healthcare disproportionately experience exhaustion, dissatisfaction, depression and burnout. In addition to the stressors of work that’s physically, emotionally and mentally demanding, in recent years there’s been the added challenge of adapting to new procedures and requirements, notably the changeover to electronic medical records and regulatory changes.
Now COVID-19 has exacerbated and put an impossible-to-ignore spotlight on the burdens that healthcare workers routinely face, report Steelcase Health researchers Jordan Smith and Seth Starner. There’s widespread awareness that the wellbeing of many healthcare workers is impaired, and strong momentum is building among their employers to make changes that can build a new culture of wellbeing within their organizations.
Some organizations already have a head start. Beginning in 2014, the healthcare profession actively addressed clinician wellbeing as the Quadruple Aim began to replace the widely recognized Triple Aim framework. This happened in response to a mounting realization that the original three aims — enhancing the patient experience, reducing costs and improving population health — simply couldn’t be achieved without also improving the work life of healthcare workers.
Setting New Priorities
So far, as healthcare organizations have begun to address the issue of staff wellbeing, “a lot of emphasis has been placed on the individual — more education and training, developing more resilience skills,” reports Smith. “And, certainly, that’s part of the answer.”
However, placing too much responsibility on the individual for their personal wellbeing — essentially telling them to “go fix yourself” — is simplistic, and can even be off-putting, says Smith.
“In reality, clinician wellbeing is multifactorial. One well documented factor contributing to clinician burnout is the need for leadership to understand and appreciate the clinician experience,” explains Starner. Yes, wellbeing involves personal resilience. But leading organizations recognize that it also depends on having the right work practices and strongly committed leadership that puts a priority on providing the necessary infrastructure and resources to steer their culture in a new, healthier direction.
One breakthrough opportunity that’s finally gaining traction is recognizing healthcare workers’ need for on-the-job respite — communicating that taking a break is not only acceptable, it’s actually important and expected.
Transforming make-do, run-of-the-mill breakrooms into thoughtfully designed respite spaces takes that message beyond words, making it tangible and much more achievable. “Space is a way to demonstrate respect,” Smith emphasizes. “An inviting, accessible respite space that meets a range of clinicians’ needs sends a message that we value you and want to make sure that you are able to function at your very best.”
Designing for Respite
Whether you’re adapting an existing space or creating a brand-new respite setting, consider these design principles to ensure you’re providing a space that offers the affordances that healthcare workers really want and need.

- Safety, always an important consideration, has become a #1 concern as a result of COVID-19. In the near term, respite spaces may require new cleaning protocols, limiting the number of people who can be there at the same time, rearranging or removing furniture, or even adding separation screens. The addition of advanced air filtration can help reduce risk and make staff feel safe without being totally encapsulated in personal protective equipment during their break.
- Flexibility is important because needs can change quickly. A break may start as a solitary moment, but the space should be able to easily morph to support spontaneous collaboration or socializing — and vice versa. Flexible zoning along with easy-to-move screens and furniture ensures a layout that can accommodate a range of activities and needs. Flexibility also means providing options that can be modified by the user, for example recliners and seating with ergonomic adjustments.
- Biophilia is an evidence-based way to reduce stress and promote a sense of comfort and calm. Adjustable lighting, nature-inspired art, colors and motifs, and sound-dampening “white noise” are all experiential elements that can satisfy people’s innate need for contact with nature. If possible, exposure to natural light and outdoor views is ideal.
- Proximity is a powerful determinant of whether or not a clinician team will consider a respite space “theirs” and, correspondingly, if it actually gets used. Ideally, every unit should have its own respite space, preferably near to where staff is working but out of the patient and family footpath to maximize opportunities for rejuvenation. In addition, consider ways to create settings for micro breaks within work settings, such as a shielded enclave adjacent to the nurse station.

The ROIs of Wellbeing
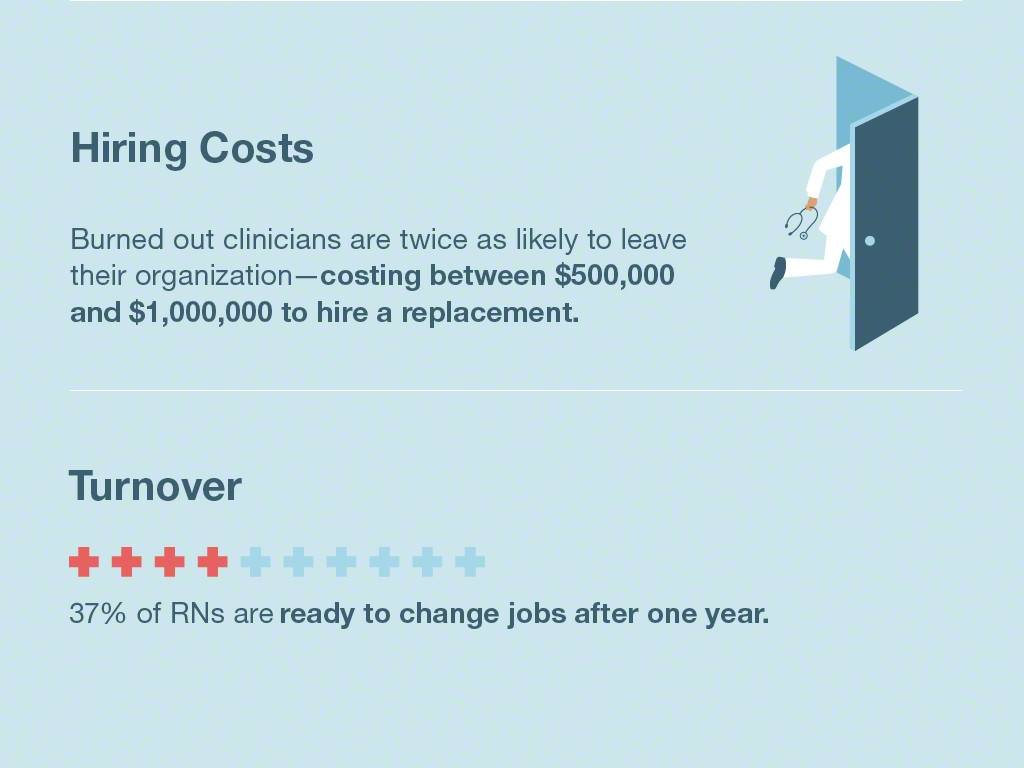
More than ever, healthcare is a profession of overburdening demands that take extreme human tolls— physically, mentally and emotionally. In today’s environment, attracting and retaining staff has become a major challenge as dissatisfaction and burnout collide with an aging-out workforce, creating serious shortages that threaten an organization’s ability to deliver optimal patient care.
Turnover carries substantial expense to health care organizations. For example, according to leading physician wellbeing researchers, the cost to replace a physician is 2 to 3 times their annual salary due to the direct costs of recruitment, as well as lost revenue during recruitment, onboarding and the time it takes for a new physician to reach optimal efficiency.*
*Shanafelt, T. D., Hasan, O., Dyrbye, L. N., Sinsky, C. A., Satele, D., Sloan, J., & West, C. P. (2015). Changes in Burnout and Satisfaction With Work-Life Balance in Physicians and the General US Working Population Between 2011 and 2014. Mayo Clinic Proceedings, 90(12), 1600–1613. http://doi.org/10.1016/j.mayocp.2015.08.023
Yes, addressing such threats requires investments, ranging from short-term improvements to longer-term solutions such as adding a chief wellbeing officer to the C-suite to tackle challenges systemically. However, investments offer substantial returns. For example, according to one calculation, assuming a 20% reduction in risk of physician burnout, investments in interventions could conservatively offer a 12.5% ROI.**
**Shanafelt, T. D., Goh, J., & Sinsky, C. A. (2017). The Business Case for Investing in Physician Well-being. JAMA Internal Medicine, 177(12), 1826–1832. http://doi.org/10.1001/jamainternmed.2017.4340
Putting a new priority on healthcare workers’ need for respite by providing appealing, thoughtful settings where it can occur is one of many steps healthcare organizations can take now to meet their benchmarks by improving the work lives of those who deliver care.
For clinician respite design solutions, visit our Planning Ideas.


